Wider use of tranexamic acid (TXA) in surgery would improve surgical outcomes, avoid unnecessary blood transfusions and conserve blood stocks, according to an article published today in the British Medical Journal.
The article, written by the UK Royal Colleges tranexamic acid in surgery implementation group – of which Ian Roberts, Professor of Epidemiology and Public Health at LSHTM, is a member – reports that, despite all the evidence, not enough is being done to ensure the availability and delivery of this inexpensive and effective drug in the UK and further afield.
Blood is a scarce resource
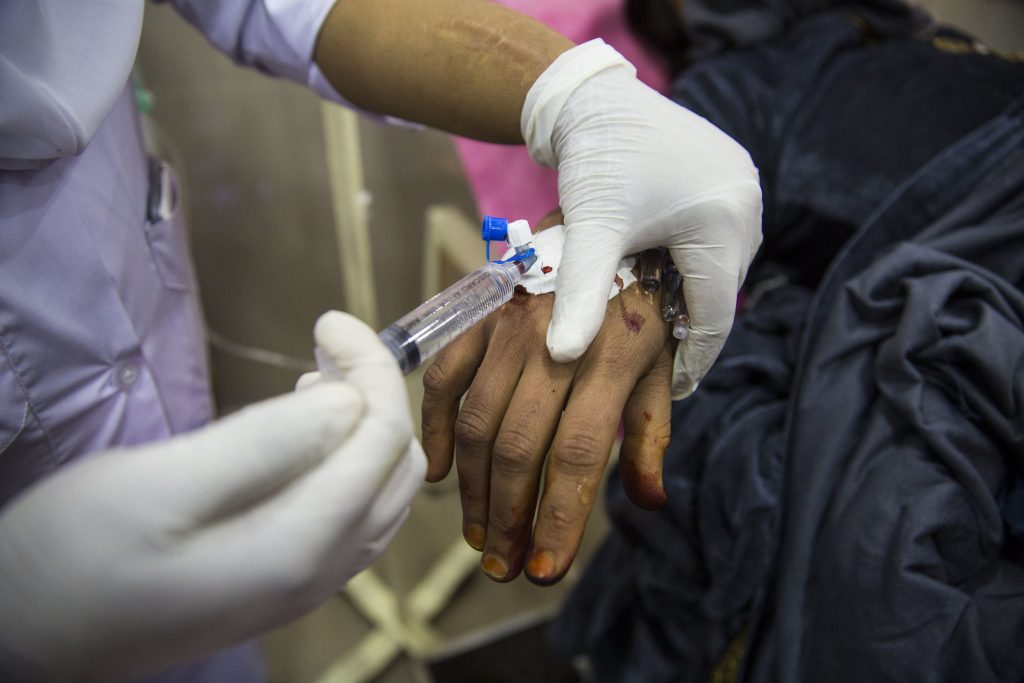
Each year, over 300 million people around the world undergo a major surgical procedure, of which around 4 million die within 30 days of the operation. Major bleeding accounts for the largest share of these deaths. Transfusions can be lifesaving, but blood is a scarce resource and there are transfusion related risks. The evidence that TXA reduces both surgical bleeding and the need for transfusion has important implications for patient care.
Professor Roberts says: “Surveys have shown that many patients want to avoid blood transfusions and, in some circumstances in the UK, surgeries are cancelled because of low blood stocks. The failure to use TXA more widely in these instances is a failure of patient care.”
The article reports that at least one third of surgical patients in the UK who should receive TXA are not treated, with half a million surgical patients in the UK missing out on its benefits. A major barrier to uptake seems to be that TXA is a generic drug which no organisation is responsible for implementing or marketing.
Tranexamic acid remains little known and underused
“With no financial incentive to create a market for the production, supply and distribution of TXA – as well as a lack of resources for large-scale education and sensitisation programmes among health bodies, clinicians, surgeons, anaesthetists, nurses, midwives and obstetricians – TXA remains hidden in the shadows and woefully underused,” said Professor Roberts.
This article comes less than a month after the Infected Blood Inquiry has ended. The Inquiry examined how more than 30,000 people in the UK contracted HIV and hepatitis after receiving infected blood and blood products between 1970 and 1990. The inquiry report, published on 20 May 2024, includes recommendations on the use of TXA.
Professor Roberts says: “The Infected Blood Inquiry, at which I gave evidence, is a huge tragedy, which should have been avoided. TXA reduces bleeding by stopping the breakdown of fibrin blood clots and has been proven to reduce the need for blood transfusion.
“In low- and middle-income countries, this is especially significant as blood stocks are not always available, not properly managed and mistakes and tragedies happen regularly. TXA is heat stable and has a long shelf life, making it cost-effective, even in low-income settings.”
An earlier 2012 systematic review produced strong evidence that TXA reduces the risk of peri-operative blood transfusion by up to one third, thus also reducing the duration of anaesthesia, the need for intensive care; and facilitating early discharge.
A further analysis of data from 50,000 and 100,000 patients also showed that using TXA did not lead to an increased risk of thrombosis. Although high doses of TXA can cause seizures, the dose given before an operation is not associated with an increased risk.
Tranexamic acid and postpartum haemorrhage
LSHTM’s Clinical Trials Unit has been working to provide evidence on the use of TXA for the treatment of postpartum haemorrhage (PPH) for over a decade.
In 2017, the WOMAN Trial found TXA reduces death from bleeding and the need for surgery to control bleeding by about one third when given to women with PPH within three hours of birth. These results led to the inclusion of TXA in the WHO guidelines for the treatment of PPH, and stimulated initiatives to increase the availability of TXA for this.
Further trials, including the WOMAN-2 Trial and the I’M WOMAN Trial are looking at using TXA to prevent PPH in anaemic women, as well as easier ways to administer TXA.
Professor Roberts added: “Based on the evidence, I believe that TXA should be included in the WHO Safe Surgery checklist. I would also urge surgeons and anaesthetists in the UK and around the world to promote its implementation to improve patient care, reduce surgical bleeding and the need for blood transfusions, and avoid preventable deaths.”